Black Death
History
- Plague has a remarkable place in history and has
had enormous effects on the development of modern civilization. Some
scholars have even suggested that the collapse of the Roman Empire may be
linked to the spread of plague by Roman soldiers returning home from
battle in the Persian Gulf in 165 .
- For centuries, plague represented disaster for
people living in Asia, Africa and Europe and because the cause of plague
was unknown, plague outbreaks contributed to massive panic in cities and
countries where it appeared.
"Black Death" or the
Great Plague
The second pandemic, widely known as
the "Black Death" or the Great Plague, originated in China in 1334
and spread along the great trade routes to Constantinople and then to Europe,
where it claimed an estimated 60% of the European population (Benedictow, 2008).
How Did the Black Death Spread?
The Black Death of the 1340s and 1350s
was, in terms of the percentage of the population lost, the worst recorded
plague in human history. It wiped out as much as a quarter of the world’s
population, probably including more than half the population of Europe, and
records suggest that it sometimes did so in a spectacularly gruesome
way—routinely covering its victims in exploding cysts and rotting their
extremities with gangrene. It was the pneumonia and not these more visible
symptoms that killed most victims, but all told, it was a terrible way to die.
The grief and horror that survivors must have felt would have been enough to
break anyone’s heart, and that’s essentially where Europe was in these years
leading up to the Renaissance—a grieving, terrified, brokenhearted continent.
Symptoms
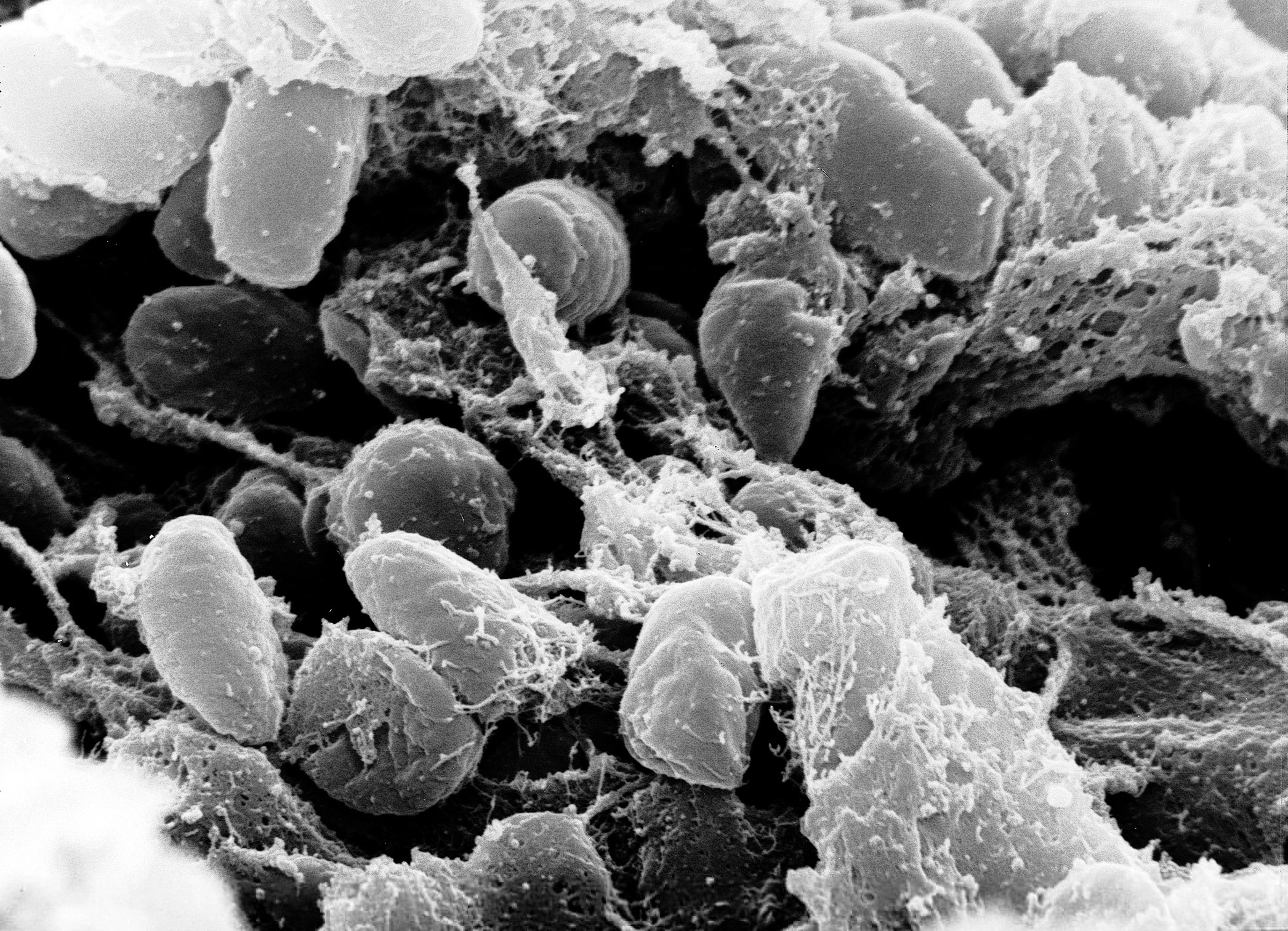
Bubonic plague affects the lymph nodes
(another part of the lymph system). Within 3 to 7 days of exposure to plague
bacteria, you will develop flu-like symptoms such
as fever,headache chills, weakness, and swollen, tender lymph glands.
How do we get ?
Usually, you get bubonic plague from
the bite of an infected flea or rodent. In rare cases, Y. pestis bacteria,
from a piece of contaminated clothing or other material used by a person with
plague, enter the body through an opening in the skin.
Treatment
When plague is suspected and diagnosed
early, a health care provider can prescribe specific antibiotics (generally
streptomycin or gentamycin). Certain other antibiotics are also effective.
Left untreated, bubonic plague bacteria
can quickly multiply in the bloodstream, causing septicemic plague, or even
progress to the lungs, causing pneumonic plague.
Prevention
Antibiotics
Health experts recommend antibiotics if
you have been exposed to wild rodent fleas during a plague outbreak in animals,
or to a possible plague-infected animal. Because there are so few cases of
plague in the United States, experts do not recommend taking antibiotics unless
it's certain a person .
References






.png)
.png)
.png)